Frequent Sports Injuries
Why the common muscle injury in athletes has become the Achilles heel for sports medicine doctors
GE and the NBA collaborate to provide doctors with clinical research to help treat common sports injuries
With the 2016 Olympics underway and team tryouts about to kick off for back-to-schoolers, late summer is the season of game time, not downtime. For elite or amateur athletes who are gearing up for competition, conditioning is key. But even the fittest among them are not without risk of injury.
From skyboxes to bleachers, fans watch the images on TV or direct from the stands – athletes in the midst of executing a critical play collapse, clutching a calf, quadricep or hamstring. It’s a sight startling enough to silence the most deafening sea of vuvuzelas. For the injured, forced to leave the game for medical attention, they await an answer, whether the injury is significant enough that it will prevent them from resuming competition.
Athletes and their fans have come to expect injuries as an unfortunate part of the game; muscle strains, tears, and pulls are the most common among them. Although most athletes have experienced some type of strain, sprain or pull, the technical term for these types of injuries is not widely known. A myotendinous injury impacts the areas where muscle transitions into tendon; it can impair performance, limit play time and can reoccur even after an athlete has healed and returned to play. Despite the prevalence of these types of injuries, very little research exists on how best to prevent and treat them. “These are basically soft-tissue injuries and these soft tissue injuries are common in all sports,” said Dr Fred Azar, chair of the research committee of the NBA Teams Physician Association. “Knowing the injury is not the issue but knowing the extent of the injury is why we need advanced research to help sort this out.”

MRI (side view) of an injured quadriceps. The site of injury shows up bright white on the left of the scan.
Typically, when athletes suffer injuries that affect the upper or lower extremities, doctors often utilize x-rays and more advanced imaging technologies such as magnetic resonance imaging (MRI) or ultra-sound. Frequently occurring in the lower limbs, myotendinous injuries account for one third of all referrals to sports doctors.¹ Hamstring injuries are the most common form of these injuries in elite athletes who engage in sudden and rapid movements such as sprinting and jumping.² And although the frequency and debilitating impact of these injuries are well recognized, evidenced-based treatment options are not.
To better serve athletes and the doctors who treat them, in collaboration, the NBA and GE Healthcare are issuing a Call for Proposals (CFP) to researchers in orthopedics, sports medicine, radiology, and related disciplines asking for research and evidence-based treatment options that, up to this point, have been largely anecdotal. “We don’t know what we can tell people to do to avoid and best treat these injuries, and we’re hoping this research can answer that,” said Dr Kimberly Harmon, sports medicine physician at University of Washington and co-chair of the CFP along with Dr Azar. “We’ve been providing treatments like icing, massage and physical therapy for 40-50 years, and they seem to work but we really don’t know. It would be helpful if there was definitive research that looked at not only speeding return to play, but also prevention of recurrent injuries.”
By funding this program, the NBA and GE Healthcare are addressing high-priority clinical questions regarding the prevention, diagnosis, and treatment of acute and overuse injuries among NBA athletes, and importantly, to apply these findings to future basketball players, other athletes, and the general population. Dr. Azar believes in this myotendinous research collaboration between the NBA and GE Healthcare: “There is a lot of research out there but the answers are elusive and there’s no consensus. By knowing this information is scaled to other elite athletes, even the youngest athletes, we can use this information to help athletes in all sports, not just basketball. It really transcends college, high school and professional sports to target the population for a broad reach.”
This is the second CFP sponsored by the NBA and GE Healthcare. The first round was dedicated to tendinopathy research.
The latest myotendinous CFP will award up to $1.5 million dollars over a three-year period to support preclinical and clinical research. More information and complete CFP instructions and application forms are available at the NBA & GE Healthcare collaboration site.
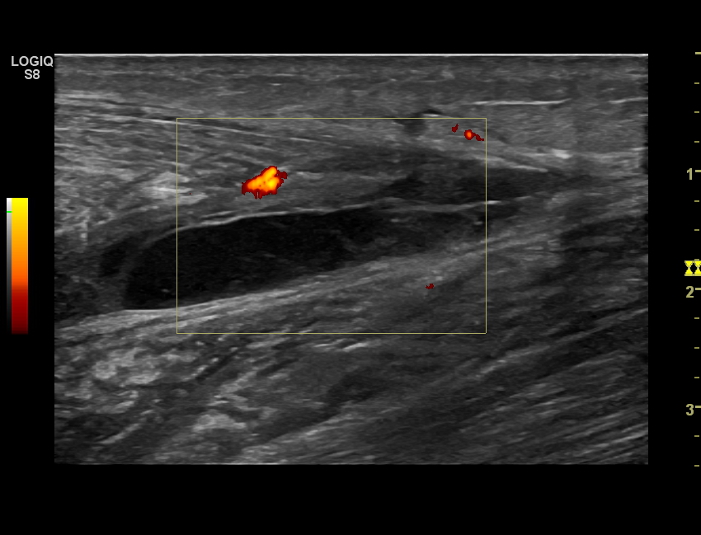
Ultrasound image: Ruptured calf muscle – image depicts a hematoma (blood clot and swelling within the tissues)
*Ultrasound photos provided by Dr. Fernando Jimenez, MD PhD, Universidad de Castilla la Mancha
¹ Krejci V, Koch P: Muscle and tendon injuries in athletes. Chicago, Yearbook Medical publishers, 1979
² Lieberman GM, Harwin SF: Pelvis, hip and thigh,: Sports medicine: principles of primary care. Mosby, 1997 pp 306-314





